Forming the Team Canada of Cancer Research

When Terry Fox set out on his Marathon of Hope in 1980, he united Canadians under a dream of a world without cancer. For over forty years, this dream has stayed alive thanks to the tireless work of patients, donors, volunteers, researchers and clinicians across the country who have all played a part in improving how we prevent, diagnose and treat cancers.
Today, this diverse group of people is more united than ever thanks to the Marathon of Hope Cancer Centres Network. This groundbreaking initiative is uniting Canadians from all walks of life to form the Team Canada of Cancer Research.
Those of us with lived experience – meaning we have received a cancer diagnosis or have cared for loved ones with cancer – are an integral part of this team. As patients, survivors, caregivers, and family members, we are, after all, the ones who can best speak to what it’s like to live with cancer. We know, better than anyone else, that there are still many gaps in cancer research, diagnosis and treatments.
This is why so many of us responded to the Network’s call to join its Patient Working Group. As part of this group, we help the Network shape its activities to reflect our needs and values. Together, we are working with clinicians, researchers and administrators from institutions across the country so that, one day, every cancer patient in Canada can receive the right treatment at the right time based on who they are as an individual and the specific characteristics of their tumour.
As we continue working towards this goal, we think that it is essential that every Canadian know what the Marathon of Hope Cancer Centres Network is doing to accelerate something called precision medicine for cancer, which you will learn more about below.
We hope this Patient Hub will answer any questions you may have regarding precision oncology and how the Marathon of Hope Cancer Centres Network is trying to make it a reality for more Canadians. We will continue to grow this Hub over time, so please check back regularly. And if there is a question that we haven’t answered, please let us know by filling out the form at the bottom of this page.
Sincerely,
The Marathon of Hope Cancer Centres Network's Patient Working Group
The Marathon of Hope Cancer Centres Network (also known as the MOHCCN or “the Network”) is a national initiative led by the Terry Fox Research Institute and the Terry Fox Foundation. It is funded by the federal government and partner institutions across the country. Inspired by Terry Fox, the Network’s main goal is to unite cancer researchers, clinicians, patients, and administrators from over 30 institutions across Canada under a single vision: to improve outcomes and quality of life of cancer patients by accelerating the implementation of precision medicine for cancer.
Just as everyone’s DNA is unique, each person’s cancer also has a distinct molecular profile. For example, two breast cancers that look similar under a microscope can be driven by different mutations, making them respond differently to treatment.
Today, cancers are most often treated according to their type and location, whereas precision medicine for cancer (also known as precision oncology) is based on the idea that an individual patient’s treatment can be guided by their unique characteristics, including their tumour’s individual molecular signature. For example, patients whose tumour cells carry a mutation in a specific gene may receive a drug that acts against that mutation, instead of a “one-size-fits-all" chemotherapy. This helps personalize treatments, so that each patient receives the right drug at the right dose at the right time.
Precision oncology aims to identify which treatment is most likely to work – or not work – against a patient’s specific cancer. This targeted, personalized approach aims to improve survival and quality of life of patients by improving the chances of a successful treatment, reducing uncertainty and diminishing the impact that unsuccessful treatments can have on a patient’s physical and emotional well-being.
Understanding the mutations that drive cancer in each patient can also help devise new tests and screening protocols to diagnose and detect cancers earlier, when they may be more treatable. In this way, precision oncology can help intercept cancers at an earlier stage, when treatments are often more effective and less disruptive to patients’ quality of life, leading to improved care experiences and overall survival.
While precision medicine holds great potential, it is still in its early days. In fact, today, it only helps a small percentage of cancer patients.
There are many reasons why this is the case. For one, we still have a lot to learn about the biology of cancer and how specific mutations affect different aspects of a cancer’s growth, its ability to evade detection from the immune system and its resistance to current therapies. We also need to better understand how each person’s individual context shapes their response to specific treatments.
To act on this knowledge, we also need to have safe and effective drugs that target the individual characteristics of each patient and their tumour. These targeted drugs exist for some cancers, but there is still a lot of work to be done to make more of these kinds of drugs available to more people.
Since precision oncology is currently applied inconsistently and in a small proportion of patients, it is difficult to study. There is much to learn about the context in which it is most effective and how it can be best applied in a way that responds to what patients want. These and many other questions about precision medicine need to be answered for more people to benefit from this promising type of cancer care.
To make precision medicine a reality for more Canadians, we need everyone involved in cancer research and care to work together. This is why the Marathon of Hope Cancer Centres Network has created the Team Canada of Cancer Research. This constantly growing group is made up of patients, researchers, oncologists, administrators and donors from across the country who are sharing data, knowledge and resources like never before to benefit all Canadian cancer patients, regardless of where they are in the country.
This unified approach is instrumental in part because answering all the remaining questions about precision medicine requires a tremendous amount of data. On their own, individual organizations simply wouldn’t have enough data needed for such intensive research. This is where the Marathon of Hope Cancer Centres Network comes in, promoting a team approach that leverages the strengths of its partner institutions and members. In the first phase of the Network, we are building the country’s largest and most complete cancer research dataset, the MOHCCN Gold Cohort. This resource will allow researchers to study how and why real-world cancer patients respond to specific drugs, and its creation is helping to build the expertise and infrastructure needed to gather, share and analyze clinical and genomic data in ways that will benefit cancer patients now and into the future.
Beyond the creation of this game-changing data generation and sharing infrastructure, the Network is building the capacity and collaborative networks needed across Canada to study and implement precision oncology at scale. This ambitious goal requires an unprecedented amount of teamwork and large investments in both people and systems, both of which are being catalyzed through the Network.



The Marathon of Hope Cancer Centres Network’s Gold Cohort seeks to be Canada’s largest and most complete cancer case resource. It will include paired clinical and genomic data from a diverse pool of 15,000 Canadian cancer patients, with different cancers, treated across the country. This resource will provide a huge amount of data that will be crucial to better understand how precision oncology can be most effectively applied to patients.
To create this resource, Network members first started working together to determine uniform ways to collect, share and analyze this patient data in ways that are scientifically rigorous and that protect the privacy of each patient involved. This essential groundwork is now allowing us to collect this data and start asking questions of it, such as what characteristics or genetic mutations make cancer patients more likely to respond to a certain drug. A handful of cases may not answer important questions like this one, but data from thousands of cancer patients will reveal key patterns.
Some people have compared this to a pointillism painting: if you look up close at one dot, it may not look like anything, but if you zoom out and observe the collection of thousands and thousands of dots, you see the full picture. The Marathon of Hope Cancer Centres Network hopes to create that full picture through the creation of the massive dataset that will be the MOHCCN Gold Cohort and the additional data sharing it will catalyze.
The guidelines, standards and policies directing this work are being created by more than a dozen Network working groups made up of experts from across the country. Strict ethical, legal, quality-control, and accessibility standards ensure that the data is scientifically useful and available for sanctioned research studies while also protecting the privacy of cancer patients. This all helps to make the Gold Cohort complete, accurate, permanent and accessible, meaning that researchers many years from now will still be able to use it to answer scientific questions that perhaps haven’t even been thought of yet. It also means that clinicians may, one day, be able to use artificial intelligence (AI) to match patients to personalized treatments based on how other patients with similar tumour characteristics responded to various treatments.
While our first goal is to have the Gold Cohort reach 15,000 cases, it is the Network’s vision that this resource will continue growing, and that one day, data from every cancer patient treated in Canada will be added to it. The more cases are entered into the system, the more accurate precision oncology becomes.
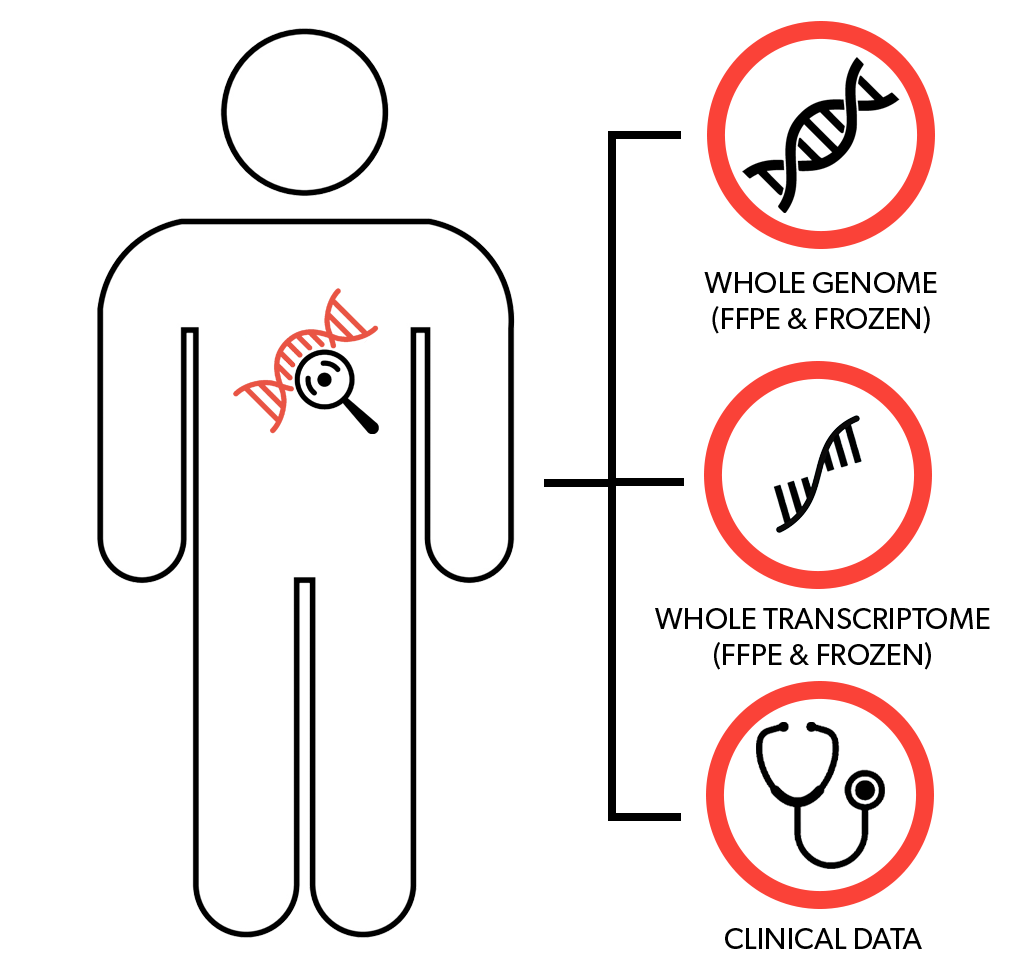
For a case to be included in the Gold Cohort, it must meet a set of minimum requirements laid out in the MOHCCN Gold Cohort Standards Policy. Currently, these requirements include both genomic and clinical data.
A standardized set of more than 100 clinical data elements, including for example the patient’s cancer diagnosis and staging information as well as what treatment(s) they received and how they responded to it (them), must be available for each patient. All clinical information is de-identified, meaning that data that could be used to identify the patient is removed or modified to make the information anonymous.
Genomic profiling of the cancer sample is also performed and must reach quality criteria. This includes profiling of DNA and, when possible, RNA extracted from tumour cells to provide a broad view of the cancer’s molecular characteristics. DNA from normal cells (usually obtained through a standard blood test) is also sequenced to help identify genetic changes that are specific to tumour cells versus those that are present in normal, non-cancerous cells (i.e. ‘germline’ alterations). Together, all of this profiling is known as whole-genome and transcriptome analysis (WGTA).
In addition to WGTA data, other data can also be included for each case, where applicable. This can include, for example, imaging data or immune profiling data. The Network is also running a competition to see what other data points would help enhance the scientific impact of the Gold Cohort.
This combination of clinical and genomic data is immensely valuable, as it allows researchers to link certain cancer behaviours, such as aggressiveness or response to treatment, to a tumour’s molecular features. This can in turn help predict how other cancers may progress or respond to various treatments.
To populate the Gold Cohort, the Marathon of Hope Cancer Centres Network is funding more than 100 projects focused on data generation in over 30 partner institutions across Canada.
These projects have been selected due to their ability to generate data according to the stringent legal, ethical and quality-control guidelines established by the Network and add both prospective (newly diagnosed) and retrospective (already diagnosed with samples available through a biobank) cases to the Gold Cohort. Informed patient consent to their samples being used in a research setting is required for all cases.
In practice, there are two main types of projects currently adding cases to the Gold Cohort: regional consortia projects and pan-Canadian projects. Regional consortia projects are approved at the consortium level (more on this below), while Pan-Canadian projects – which bring together researchers from across the country – were awarded after an expert review panel assessed applications submitted through a call for proposals.
As we continue to implement our standards and build the infrastructure needed to collect, curate and share data across the country, it is the Network’s vision to expand beyond this current model, so that any patient across the country wanting to donate their data to the Network will be able to easily enroll in an MOHCCN-supported study to do so.
The Marathon of Hope Cancer Centres Network is anchored by five regional consortia (a group of institutions from a particular region that have agreed to work together to achieve a common goal) representing all ten provinces. From west to east, these are: the BC Cancer Consortium (BC2C), the Prairies Cancer Consortium (PR2C), the Princess Margaret Cancer Consortium (PM2C), the Marathon of Hope - Québec (MOH-Q) consortium, and the Atlantic Cancer Consortium (ACC). Each consortium is composed of member sites and partnered with academic, research, and health institutions.
Member institutions are those that signed the MOHCCN Network Master Agreement or a Joinder Agreement with the Terry Fox Research Institute. This is a pre-requirement to receive a grant for Network activities. Network Partners, on the other hand, participate or collaborate on certain Network activities and may have researchers associated with the Network, but are not Network Members. Partners may have an official agreement with a Network Member, but no official agreement with the Network itself.
Individuals can also become Network members. This can be done through several avenues, such as leading or participating in a Network-funded project or a project contributing cases to the Gold Cohort, or being a member of one of the Network’s working groups. Network members therefore include researchers, clinicians, patients and caregivers, project managers, administrators, and more!

Membership of the Marathon of Hope Cancer Centres Network in July 2024.
The Government of Canada, through Health Canada, is investing up to $150 million to fund the Marathon of Hope Cancer Centres Network. This investment must be matched dollar-for-dollar by the Network, from sources that include the Terry Fox Foundation, foundations affiliated with member institutions, other philanthropic organizations and non-federal research funding groups. Together, this positions the Network as an unprecedented collaboration worth up to $300 million in new funds for precision oncology research
The Marathon of Hope Cancer Centres Network is led by Executive Director Dr. André Veillette and governed by a Network Council composed of leaders from member institutions, a representative of the Patient Working Group, TFRI leadership and observers from Health Canada, the Canadian Institutes of Health Research (CIHR) and the Terry Fox Foundation.
More than a dozen expert working groups have been formed, with members from all consortia, to develop standards, policies and guidelines to help direct Network operations and ensure alignment across centres. A steering committee composed of consortia leads and chairpersons from the working groups provides operational guidance.
The Network also has an External Scientific Advisory Committee, made up of world-class scientific experts from outside the Network, that provides scientific and administrative guidance.
The Marathon of Hope Cancer Centres Network has five main funding priorities:
One of the goals of the Network is to create a rich dataset of paired genomic and clinical information from patients across a wide range of cancer types and backgrounds to help facilitate precision oncology research to benefit all Canadian cancer patients. This dataset, which we are calling the Gold Cohort, will be composed of 15,000 cancer cases and promises to be among the most comprehensive cancer resources ever assembled.
We believe that precision oncology is the future of cancer care in Canada. To help make this a reality, the Network is investing in the next generation of experts in the field. Through funding and mentorship, the MOHCCN Clinician-Scientist Awards and the MOHCCN Health Informatics & Data Scientist Awards support early-career researchers specializing in different fields within precision oncology.
This funding opportunity aims to support research studies that centre patients, caregivers, and survivors and their needs as it relates to precision cancer research and care. It is driven by research themes identified by the Network’s Patient Working Group and has a goal of amplifying patient voices and priorities to elevate the quality and impact of cancer research in Canada.
The MOHCCN is also funding special initiatives and projects to ensure that advances in precision oncology reach those who need it most. For example, the Network is funding programs such as the Northern Biobank Initiative (NBI) to ensure that data generated through the Network is representative of the Canadian population and will help enable solutions that are inclusive, representative and fair. We are also funding health technology assessment (HTA) projects that investigate economic and social aspects of precision oncology, including questions of equitable access.
Data generated through the Gold Cohort will play a vital role in precision oncology research, both in Canada and worldwide. Facilitating this will require the deployment of innovative new technology and methods across the country to support data generation, sharing and analysis. Funding from the Network is helping to develop a novel data ecosystem, along with tools that allow researchers to view and access the Network’s data for precision oncology studies.
Do you have unanswered questions? Is there anything we need to add to this Patient Hub? Fill out the form and let us know! [PLEASE NOTE: You will receive a confirmation email after filling our the form. We will do our best to answer in a timely manner.]
Hear directly from the patients who are helping to build the Team Canada of Cancer Research.
Here are some of the most exciting developments from the Marathon of Hope Cancer Centres Network.
Learn more about how the Network is tackling key issues in precision medicine directly from the clinicians, researchers, data specialists and administrators who make up the Team Canada of Cancer Research.
Conversations between cancer patients and other members of the Marathon of Hope Cancer Centres Network.




The MOHCCN Patient Working Group is made up of 30 individuals from 9 provinces who are cancer patients, survivors, family members and caregivers.
Together with other members of the Team Canada of Cancer Research, we are working to ensure that all Network activities are helping to advance precision medicine in ways that are aligned with the values and desires of cancer patients.
